
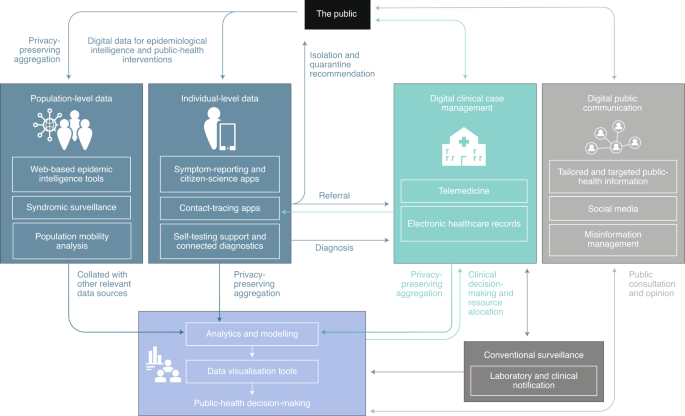
Digital technologies are being harnessed to support the public-health response to COVID-19 worldwide, including population surveillance, case identification, contact tracing and evaluation of interventions on the basis of mobility data and communication with the public. These rapid responses leverage billions of mobile phones, large online datasets, connected devices, relatively low-cost computing resources and advances in machine learning and natural language processing. This Review aims to capture the breadth of digital innovations for the public-health response to COVID-19 worldwide and their limitations, and barriers to their implementation, including legal, ethical and privacy barriers, as well as organizational and workforce barriers. The future of public health is likely to become increasingly digital, and we review the need for the alignment of international strategies for the regulation, evaluation and use of digital technologies to strengthen pandemic management, and future preparedness for COVID-19 and other infectious diseases.


COVID-19, a previously unknown respiratory illness caused by the coronavirus SARS-CoV-2 1,2 , was declared a pandemic by the World Health Organization (WHO) on 11 March 2020, less than 3 months after cases were first detected. With now over 9.8 million confirmed cases and more than 495,000 deaths 3 recorded worldwide, there are grave concerns about the global health, societal and economic effects of this virus, particularly on vulnerable and disadvantaged populations, and in low- and middle-income countries with fragile health systems 4,5 . At the time of this writing, 7.1 billion people live in countries that have had substantial travel and social restrictions 6 .
As with the control of outbreaks and pandemics before it, controlling the COVID-19 pandemic rests on the detection and containment of clusters of infection and the interruption of community transmission to mitigate the impact on human health. During the plague outbreak that affected 14th-century Europe, isolation of affected communities and restriction of population movement were used to avoid further spread 7 . These public-health measures for outbreak response remain relevant today, including surveillance, rapid case identification, interruption of community transmission and strong public communication. Monitoring how these measures are implemented and their impact on incidence and mortality is essential.
All countries are required by the International Health Regulations (2005) 8 to have core capacity to ensure national preparedness for infectious hazards that have the potential to spread internationally. Research and development of new methods and technologies to strengthen these core capacities often occurs during outbreaks, when innovation is an absolute necessity 9 . During the outbreak of severe acute respiratory syndrome in 2003, Hong Kong identified clusters of disease through the use of electronic data systems 10 . During the Ebola outbreaks in West Africa in 2014–2016, mobile phone data were used to model travel patterns 11 , and hand-held sequencing devices permitted more-effective contact tracing and a better understanding of the dynamics of the outbreaks 12 . Similarly, digital technologies also have been deployed in the COVID-19 pandemic 13,14 (Table 1) to strengthen each of the four public-health measures noted above.

A core public-health function of outbreak management is understanding infection transmission in time, place and person, and identifying risk factors for the disease to guide effective interventions. A range of digital data sources are being used to enhance and interpret key epidemiological data gathered by public-health authorities for COVID-19.
Established population-surveillance systems typically rely on health-related data from laboratories, notifications of cases diagnosed by clinicians and syndromic surveillance networks. Syndromic surveillance networks are based on reports of clinical symptoms, such as ‘influenza-like illness’, rather than a laboratory diagnosis, from hospital and selected sentinel primary and secondary healthcare facilities, which agree to provide regular surveillance data of all cases. These sources, however, ultimately miss cases in which healthcare is not sought. In the UK, for example, where until recently only hospitalized patients and healthcare workers were routinely tested for COVID-19, confirmed cases represent an estimated 4.7% of symptomatic COVID-19 cases 18 . Identifying undetected cases would help elucidate the magnitude and characteristics of the outbreak 19 and reduce onward transmission.
In the past two decades, data from online news sites, news-aggregation services, social networks, web searches and participatory longitudinal community cohorts have aimed to fill this gap. Data-aggregation systems, including ProMED-mail 20 , GPHIN 21 , HealthMap 22 and EIOS 23 , which use natural language processing and machine learning to process and filter online data, have been developed to provide epidemiological insight. These data sources are increasingly being integrated into the formal surveillance landscape 24 and have a role in COVID-19 surveillance. The WHO’s platform EPI-BRAIN brings together diverse datasets for infectious-disease emergency preparedness and response, including environmental and meteorological data 25 . Several systems have claimed detection of early disease reports for COVID-19, through the use of crowdsourced data and news reports, before the WHO released a statement about the outbreak 14,20,26 . The UK’s automatic syndromic surveillance system scans National Health Service digital records 27 to pick up clusters of a respiratory syndrome that could signal COVID-19. There is also interest in using online data to estimate the true community spread of infectious diseases 28,29 . Preliminary work on the epidemiological analysis of COVID-19-related social-media content has been reported 30,31,32 . Models for COVID-19 (ref. 33 ), building on previously established internet search algorithms for influenza 34 , are included in Public Health England’s weekly reports 35 .
Crowdsourcing systems used to elucidate the true burden of disease are also supporting syndromic surveillance. InfluenzaNet gathers information about symptoms and compliance with social distancing from volunteers in several European countries through a weekly survey 36 . Similar efforts exist in other countries, such as COVID Near You 37 in the USA, Canada and Mexico. The COVID-19 symptom-tracker app has been downloaded by 3.9 million people in the UK and USA 38 and is feeding into national surveillance. While rapid and informative, these systems can suffer from selection bias, over-interpretation of findings and lack of integration with official national surveillance that report established surveillance metrics. A fragmented approach has meant that there are 39 initiatives in the UK alone that are collecting symptoms from people in the community, with no centralized data collection (M. Edelstein, personal communication).
Data dashboards are being used extensively in the pandemic, collating real-time public-health data, including confirmed cases, deaths and testing figures, to keep the public informed and support policymakers in refining interventions 39,40,41 . COVID-19 dashboards typically focus on time-series charts and geographic maps, ranging from region-level statistics to case-level coordinate data 40,42 . Several dashboards show wider responses to the pandemic, such as clinical trials 43 , policy and economic interventions 44 and responses to social-distancing directives 45 . Few dashboards include data on contact tracing or community surveillance from apps or their effectiveness. Challenges with the quality and consistency of data collection remain a concern. Lack of official standards and inconsistencies in government reporting of statistics across countries make global comparisons difficult. Up-to-date and accurate offline statistics from governments are also not always accessible. Novel visualization approaches are emerging, such as the NextStrain open repository, which presents viral sequence data to create a global map of the spread of infection 41 . This is enabled by open sharing of data and is based on open-source code. Such speed of the sharing of such data has not been witnessed in previous global outbreaks 46 .
Early and rapid case identification is crucial during a pandemic 47 for the isolation of cases and appropriate contacts in order to reduce onward spread and understand key risks and modes of transmission. Digital technologies can supplement clinical and laboratory notification, through the use of symptom-based case identification and widespread access to community testing and self testing, and with automation and acceleration of reporting to public-health databases.
Case identification by online symptom reporting, as seen in Singapore 48 and the UK 49 , is traditionally used for surveillance, but it now offers advice on isolation and referrals to further healthcare services, such as video assessments 50 and testing. These services can be rapidly implemented but must be linked to ongoing public-health surveillance and to action, such as isolation of cases and quarantining of contacts. Although this approach is suitable for symptomatic people, widespread testing of people and populations, as well as contact tracing, has a crucial role in case identification, as an estimated 80% of COVID-19 cases are mild or asymptomatic 19 . Sensors, including thermal imaging cameras and infrared sensors, are being deployed to identify potential cases on the basis of febrile symptoms (for example, at airports). The large numbers of false-positive and false-negative results mean that this is unlikely to have a substantial effect beyond increasing awareness 51,52 . Wearable technologies are also being explored for monitoring COVID-19 in populations 53 .
There has been increasing interest in decentralized, digitally connected rapid diagnostic tests to widen access to testing, increase capacity and ease the strain on healthcare systems and diagnostic laboratories 54,55,56 . Several point-of-care COVID-19 PCR tests are in development 57,58 ; however, their use is still limited to healthcare settings. Drive-through testing facilities and self-swab kits have widened access to testing. There are inherent delays between sampling, sending samples to centralized labs, waiting for results and follow-up. By contrast, point-of-care rapid diagnostic antibody tests could be implemented in home or community or social-care settings and would give results within minutes. Linking to smartphones with automatic readout through the use of image processing and machine-learning methods 59,60 could allow mass testing to be linked with geospatial and patient information rapidly reported to both clinical systems and public-health systems and could speed up results. For this to work effectively, standardization of data and integration of data into electronic patient records are required.
Identifying past infections by antibody testing is also central to population-level surveillance and evaluating the efficacy of interventions such as social distancing. So far, point-of-care serology tests in particular have variable performance, and in light of the possibility that antibody responses may be short-lived, how such testing can assist in patient management remains unclear 61,62,63 . Some have argued that seropositive workers who must remain active in the economy could receive a digital ‘immunity passport’ to demonstrate protection from infection, although such a strategy is fraught with operational and clinical uncertainty 63,64 . Machine-learning algorithms are also being developed for case identification by automated differentiation of COVID-19 from community-acquired pneumonia through the use of hospital chest scans by computerized tomography 65,66,67 . Further evaluation of their utility is recommended 68,69 .
After case identification and isolation, rapid tracing and quarantining of contacts is needed to prevent further transmission 70 . In areas of high transmission, the implementation and monitoring of these interventions is needed at a scale that is becoming increasingly unfeasible or at least challenging by traditional means 71 .
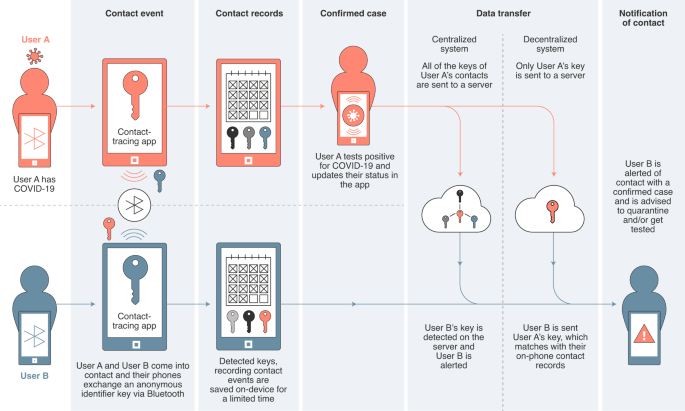
Digital contact tracing automates tracing on a scale and speed not easily replicable without digital tools 71 . It reduces reliance on human recall, particularly in densely populated areas with mobile populations. In the COVID-19 pandemic, digital contact-tracing apps have been developed for use in several countries; these apps rely on approaches and technologies not previously tried on this scale and are controversial in terms of privacy. Evaluating their accuracy and effectiveness is essential.
Early digital tracing initiatives raised concerns about privacy 72 . In South Korea, contacts of confirmed cases were traced through the use of linked location, surveillance and transaction data 73 . In China, the AliPay HealthCode app automatically detected contacts by concurrent location and automated the enforcement of strict quarantine measures by limiting the transactions permitted for users deemed to be high risk 74,75 . More-recent voluntary contact-tracing apps have been launched in collaboration with governments; these collect location data by global positioning system (GPS) or cellular networks 76 , proximity data collected by Bluetooth 72,77 or a combination of those 78,79 . Concerns have been raised about centralized systems (Fig. 2) and GPS tracking. Norway halted the use of and data collection from its Smittestopp app after the country’s data-protection watchdog objected to the app’s collection of location data as ‘disproportionate to the task’, and they recommended a Bluetooth-only approach 80 . Several international frameworks with varying levels of privacy preservation are emerging, including Decentralized Privacy-Preserving Proximity Tracing 81 , the Pan-European Privacy-Preserving Proximity Tracing initiative 82 and the joint Google–Apple framework 83 .
Aggregated location data collected by smartphones via GPS, cellular network and Wi-Fi can monitor real-time population flows 84 , identify potential transmission hotspots and give insight into the effectiveness of public-health interventions such as travel restrictions on actual human behavior. Access to mobility data is a major challenge, and these approaches have raised ethical and privacy concerns 85 .
Mobility data with privacy-preserving aggregation steps have recently been made available by several technology and telecom companies for the purposes of COVID-19 control; however, the datasets are limited and there is no long-term commitment in place for data sharing. Daily aggregated origin-destination data from Baidu 86 are being used to evaluate the effect of travel restrictions 87 and quarantine measures 88 on COVID-19 transmission in China. Analysis of the location data of Italian smartphone users estimated a reduction of 50% in the total trips between Italian provinces in the week after the announcement of lockdown on 12 March 2020 (ref. 89 ). Google has released weekly mobility reports with sub-national granularity, including breakdown by journey type and destination (such as workplaces and parks), and has made their dataset publicly downloadable 90 . Apple has similarly released a dataset with daily figures for mobility and assumed method of transport 91 . There is no standardization of these datasets between providers, however, and not all countries or regions are included in these datasets.
Assessing local differences in mobility and contact patterns may be critical for predicting the heterogeneity of transmission rates between different communities and in different regions in which household size and age-stratified contact patterns may differ. This contextual information can provide insight into the effect of interventions to slow transmission, including the impact of handwashing 92 , social distancing and school closures 93 . The monitoring of social-distancing measures could also be used to forecast health-system demands 94 and will be important in assessing the easing of restrictions when appropriate. Concerns have been raised over breaches of civil liberties and privacy when people are tracked to monitor adherence to quarantine and social distancing, including the use of wearable devices 95 and drones 96 .
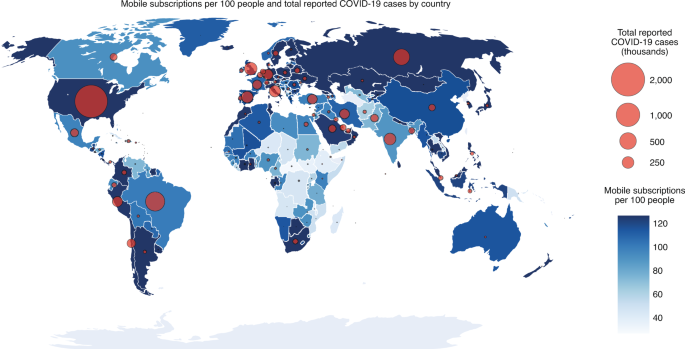
Effective implementation of interventions during a pandemic relies on public education and cooperation, supported by an appropriate communications strategy that includes active community participation to ensure public trust. With 4.1 billion people accessing the internet 97 and 5.2 billion unique mobile subscribers 15 , targeted communication through digital platforms has the potential to rapidly reach billions and encourage community mobilization (Fig. 3). Key challenges persist, including the rise of potentially harmful misinformation 98,99 and digital inequalities 100 (discussed below).
Online data and social media have had an ongoing, important role in public communication 101 since the first reports of an unusual influenza-like illness resistant to conventional treatment methods emerged in China 102 . Public-health organizations and technology companies are stepping up efforts to mitigate the spread of misinformation 103,104 and to prioritize trusted news sites; for example, Google’s SOS alert intervention 105 prioritizes the WHO and other trusted sources at the top of search results. There are few reports about the impact of these interventions 106,107 and difficulties in defining misinformation 108 . A United Nations study found that 86% of member states had placed COVID-19 information on national websites by early April 2020 (ref. 109 ), and many are using text messaging to reach populations who do not have access to the internet. Chat-bots are also providing information to reduce the burden on non-emergency health-advice call centers 110 , and clinical practice is being transformed by the rapid adoption of remote health-service delivery, including telemedicine, especially in primary care 50
Digital communication platforms are also supporting adherence to social-distancing measures. Video conferencing is allowing people to work and attend classes from home 111 , online services are supporting mental health 112 and digital platforms are enabling community-mobilization efforts by providing ways to assist those in need 113 . Nevertheless, the security and privacy of freely available communication platforms remains a concern, particularly for the flow of confidential healthcare information.
Digital technologies join a long line of public-health innovations that have been at the heart of disease-prevention-and-containment strategies for centuries. Public health has been slower to take up digital innovations than have other sectors, with the first WHO guidelines on digital health interventions for health-system strengthening published in 2019 (refs. 114,115 ). The unprecedented humanitarian and economic needs presented by COVID-19 are driving the development and adoption of new digital technologies at scale and speed. We have highlighted the potential of digital technologies to support epidemiological intelligence with online datasets, identify cases and clusters of infections, rapidly trace contacts, monitor travel patterns during lockdown and enable public-health messaging at scale. Barriers to the widespread use of digital solutions remain.
Digital technologies cannot operate in isolation and need to be integrated into existing public healthcare systems 116 . For example, South Korea and Singapore successfully introduced contact-tracing apps to support large teams of manual contact tracers as one of many measures, including strict isolation of cases and quarantine 73 .
Digital data sources, like any data source, need to be integrated and interoperable, such as with electronic patient records. Analysis and use of these data will depend on the digital infrastructure and readiness of public-health systems, spanning secondary, primary and social-care systems. The logistics of delivery to ensure population impact are often given too little attention and can lead to over-focus on the individual technology and not its effective operation in a system. The coordination of interventions is also a challenge, with multiple symptom-reporting sites in a single country, which risks fragmentation.
Looking ahead, there is a need for a systems-level approach for the vision of the ideal fit-for-purpose digital public-health system 117 that links symptom-tracking apps, rapid testing and case isolation, contact tracing and monitoring of aggregated population-mobility levels, access to care and long-term follow-up and monitoring, with public communication (Fig. 4). These types of integrated online care pathways are not new concepts, having been shown to be highly acceptable and feasible for other infectious diseases, such as chlamydia 118 .
Big-data and artificial-intelligence approaches are only as good as the empirical datasets that are put into them, yet detailed public-health and private datasets are often inaccessible, due to privacy and security concerns, and often lack standardized formats or are incomplete. Researchers are calling for technology and telecom companies to share their data in a ‘proportionate, ethical and privacy-preserving manner’ 85,119,120 , often citing a moral imperative for these companies to contribute where there is justification for data use. Some companies are making subsets of aggregated data available 86,90,91,121,122 . These data are not consistent and are not provided within the same timeframe, and there is no standard format or long-term commitment. Researcher-led international collaborations have aimed to aggregate multiple international data sources of voluntarily reported information 41,123 .
Equally, governments should provide much greater transparency in their datasets, including epidemiological data and risk factors for acquisition, with downloadable formats for researchers. Several governments have made available de-personalized individual-level datasets for research purposes 124,125 , although this raises potential privacy concerns. Open-source data, code and scientific methods are being rapidly and widely shared online, including increased use of preprints, which speed up data availability but lack peer review 126 .
Evidence of the effectiveness of any new technology is needed for wider adoption, but as the current pandemic is ongoing, many digital technologies have not yet been peer-reviewed, been integrated into public-health systems, undergone rigorous testing 127 or been evaluated by digital health-evidence frameworks, such as the evidence standards framework for digital health technologies of the National Institute for Health and Care Excellence 128 . Contact-tracing apps have been launched in at least 40 countries 129 , but there is currently no evidence of the effectiveness of these apps 130 , such as the yield of identified cases and contacts, costs, compliance with advice, empirical estimates of a reduction in the R value or a comparison with traditional methods. Although it is challenging, due to the urgency of the pandemic, evaluation of the effectiveness of interventions is essential. Researchers, companies and governments should publish the effectiveness of their technologies in peer-reviewed journals and through appropriate clinical evaluation.
There is an urgent need for coordinated international digital public-health strategies, but these have been slow to emerge. On 22 March 2020, the WHO release a draft of its global strategy on digital health for 2020–2024 (ref. 131 ). On 8 April, the European Union called for a pan-European approach on the use of apps and mobile data for COVID-19 82,132 .
Highly granular or personal data for public-health surveillance raises legal concerns 133 , ethical concerns 134,135 and security and privacy concerns 136 . Not all digital interventions have allowed consensual adoption or have made the option of consent for specific purposes explicit 75 , and some have been used to enforce measures as well as to monitor them. In many cases, widespread adoption is related to effectiveness, which highlights the need for public trust and engagement. There is concern that emergency measures set precedent and may remain in place beyond the emergency, which will lead to the ongoing collection of information about private citizens with no emergency-related purpose 137,138 . All systems will need to be ‘proofed’ against invasions of privacy and will need to comply with appropriate legal, ethical and clinical governance 75 . Data can be shared under a legal contract for a well-defined purpose and time, with requirements for independent audit 139 to ensure data are not used for purposes outside of the pandemic. Dynamic consent processes could also allow users to share their data, and privacy-preserving technologies, such as differential privacy and homomorphic encryption, could ensure that access is possible only for specific purposes and is available in a tamper-proof manner 13,140 to allow auditing.
In 2018, the World Health Assembly Resolution on Digital Health recognized the value of digital technologies in advancing universal health coverage and the Sustainable Development Goals. Although trends are narrowing, today there remains a digital divide, and 51% of the world’s population does not subscribe to the mobile internet 15 . The lack of access to mobile communications is seen in low- and middle-income countries, although people with lower socio-economic status in high-income countries are also affected 141 . The Pew Research Center reported large disparities between people 18–29 years of age and those over 50 years of age in their mobile-communication access 142 . There are also reports of restricted mobile internet access, such as in areas of Myanmar, which have left some populations unware of the pandemic 143 . This outbreak has also disproportionately affected some communities, such as Black and minority ethnic groups, more than others 144 . It is therefore essential to develop tools and messaging that are accessible 100 and can be tailored to specific risks, languages and cultural contexts.
The spread of the COVID-19 pandemic has exposed the need for government leadership to accelerate the evaluation and adoption of digital technologies. Successful implementation strategies will require carefully accelerated and coordinated policies, with collaboration among multiple areas of governments, regulators, companies, non-governmental organizations and patient groups. Public health has long been under-funded compared with the funding of other areas of health 145 . Long-term changes will necessitate investment in national and international digital centers of excellence, with the necessary balance of partners and pre-agreed access to digital datasets. A substantial investment in workforce education and skills is essential for growing digital public-health leadership 146 .
The COVID-19 pandemic is ongoing, and it is too early to fully quantify the added value of digital technologies to the pandemic response. While digital technologies offer tools for supporting a pandemic response, they are not a silver bullet. The emerging consensus is that they have an important role in a comprehensive response to outbreaks and pandemics, complementing conventional public-health measures, and thereby contribute to reducing the human and economic impact of COVID-19. Cost-effectiveness and sustainability will require systems-level approaches to building digital online care pathways that link rapid and widespread testing with digital symptom checkers, contact tracing, epidemiological intelligence and long-term clinical follow up. The COVID-19 pandemic has confirmed not only the need for data sharing but also the need for rigorous evaluation and ethical frameworks with community participation to evolve alongside the emerging field of mobile and digital healthcare. Building public trust through strong communication strategies across all digital channels and demonstrating a commitment to proportionate privacy are imperative 147 .
The future of public health is likely to be increasingly digital, and recognizing the importance of digital technology in this field and in pandemic preparedness planning has become urgent. Key stakeholders in the digital field, such as technology companies, should be long-term partners in preparedness rather than being partners only when emergencies are ongoing. Viruses know no borders and, increasingly, neither do digital technologies and data. There is an urgent need for alignment of international strategies for the regulation, evaluation and use of digital technologies to strengthen pandemic management and future preparedness for COVID-19 and other infectious diseases.